
The Quality Interactions webinar, "When Language Barriers Lead to Poor Patient Care (And What to Do About It)," provides information and care tips for successfully working with interpreters to deliver high-quality healthcare to patients with Limited English Proficiency (LEP).
A Case for Improving Care
In the webinar presentation, Dr. Alexander Green, a QI co-founder and expert in culturally competent care, provides data showing why improving healthcare services for the 25 million people in the US with LEP is so important. For example, patients with LEP receive less preventive care, have worse control of chronic conditions, and are less likely to understand their disease and treatment plans than individuals without LEP. Patients with LEP are also:
- More frequently and severely affected by adverse events
- More likely to experience medical errors due to poor communication
- More likely to suffer from physical harm when errors occur
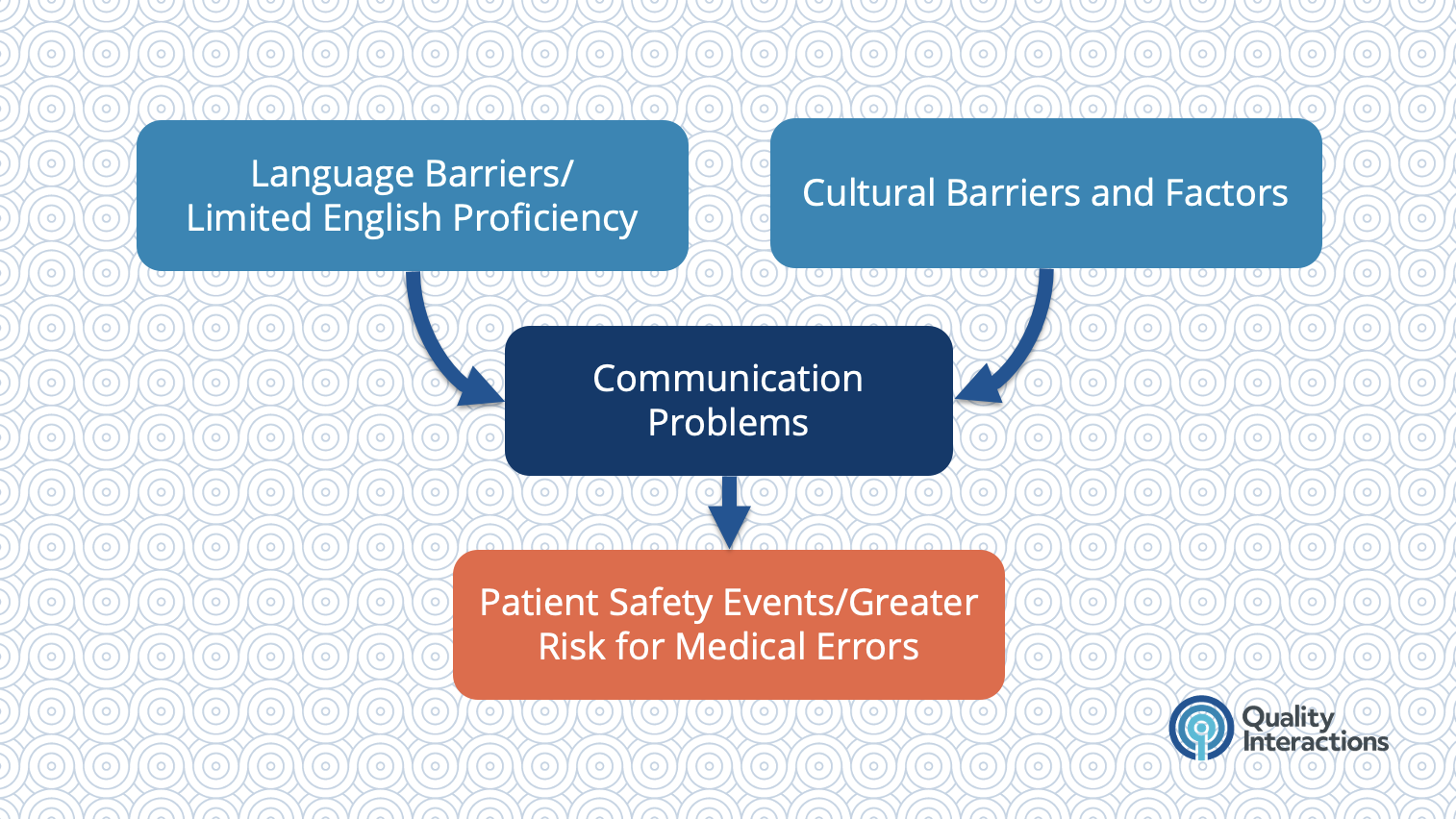
This elevated risk comes primarily from communication problems arising from language barriers and cultural factors.
Common Causes of Communication Problems with Patients with LEP
Many organizations and individual practitioners rely on ad hoc interpreters, or untrained people who are interpreting on the fly, to help communicate with patients with LEP. Examples of ad hoc interpreters include:
- A family member
- A bilingual staff member pulled away from other duties to interpret
- A self-declared bilingual in a hospital waiting room who volunteers to interpret
- An advanced language student
Dr. Green shows that ad hoc interpreters should only be used in emergencies when there is no time to arrange for a trained medical interpreter. Individuals who lack experience translating medical terminology can exacerbate communication problems and create confusion. Furthermore, there are ethical reasons to avoid involving family members—and it is illegal to ask a minor to interpret except in emergency situations.
Working with Medical Interpreters
- Convert the message
- Clarify the message
- Clarify cultural nuances
- Expanded role as patient advocates, safety monitors, and navigators

If a patient or the patient's family is resistant to using an interpreter, Dr. Green recommends respectfully asserting the need for professional medical interpretation. For example:
“Even though you do speak English, I need to make sure that there are no miscommunications or mistakes made.”
“Even though your family member wants to interpret, professional interpreters are trained to understand medical terminology ensure that we don’t miss anything important.”
“This is the policy of the clinic/hospital/practice.”
Dr. Green's 5 Tips for Working with Medical Interpreters
- Prepare for the encounter - ideally, meet briefly with the interpreter to go over the patient's history and goals for the interaction
- Set the stage - if in person, arrange the chairs in a triangle shape so everyone can make eye contact
- Keep it simple - avoid medical jargon and use short sentences
- Pay attention to nonverbal cues - watch your patient for body language and tone
- Debrief and document - discuss the interaction with the interpreter afterward and ask for clarification if necessary
Questions & Answers
Many participants in the webinar had specific questions about improving care for patients with LEP. In this blog post, Dr. Green responds to the questions he didn't have time to address during the live presentation.

