Active listening is one of the most effective tools in clinical care, but it is often overlooked. Time constraints and high patient volume can shift provider focus to efficiency rather than connection. But genuine listening remains one of the most powerful ways to build trust, improve understanding, and boost patient outcomes.
Why active listening matters in healthcare
Active listening is more than a communication skill. It is a clinical competency that directly influences quality of care. Research shows that when physicians allow patients to share their story without interruption, the average time before patients stop talking is less than 90 seconds, yet those brief moments often reveal critical details that guide diagnosis and treatment.
Patients who feel heard are more likely to provide accurate information, adhere to treatment plans, and report higher satisfaction with their care. Studies also link active listening to improved patient safety and fewer communication-related errors, underscoring its essential role in clinical practice.
How to practice active listening in clinical settings
Active listening requires intention and focus. It involves more than hearing words; it means understanding meaning, emotion, and context. In practice, clinicians can strengthen their listening skills by:
-
Showing attention: Maintain eye contact, silence devices, and minimize distractions to signal focus.
-
Listening for meaning: Observe tone, hesitation, and nonverbal cues that reveal unspoken concerns.
-
Clarifying with curiosity: Ask open-ended questions to confirm understanding instead of making assumptions.
-
Validating emotion: Acknowledge feelings without judgment to foster trust and openness.
-
Ensuring shared understanding: Summarize next steps in plain language and invite questions before concluding the visit.
Each of these actions helps patients feel respected and improves the accuracy of clinical communication.
The impact of active listening on patient outcomes
Evidence consistently shows that active listening leads to better outcomes across clinical environments. One study found that physicians who listen attentively and empathetically experience higher patient satisfaction scores and improved adherence rates. Other research indicates that active listening strengthens the patient–provider relationship, leading to more effective care coordination and fewer missed diagnoses.
Clinicians also benefit. Listening with presence and curiosity reduces stress, increases professional satisfaction, and promotes a sense of connection that counteracts burnout. Within care teams, active listening improves collaboration and reduces communication errors, reinforcing safety and efficiency.
Strategies for building stronger listening habits
Like any skill, active listening improves with practice and awareness. Clinicians can start with small, intentional changes:
-
Pause before responding. Allow silence to encourage patients to elaborate.
-
Reflect what you hear. Use phrases such as “It sounds like your main concern is…” to confirm understanding.
-
Check comprehension. Use the Teach-Back method to ensure that patients understand and agree on next steps.
These techniques require little additional time but can significantly improve communication and outcomes.
Improving communication and connection in care
Active listening strengthens the foundation of patient-centered care. Giving patients undivided attention and responding with empathy and clarity improves diagnostic accuracy and also enhances patient trust and satisfaction.
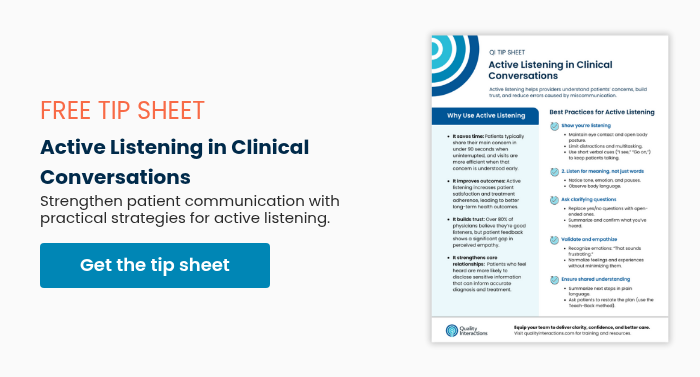
Download our Active Listening in Clinical Conversations tip sheet for a concise summary of best practices and practical strategies to apply in daily clinical interactions.
You may also like: